Just what the doctor ordered
An innovative social prescribing initiative may help alleviate some of the social burden placed on health care providers and provide much-needed support for Ontarians.
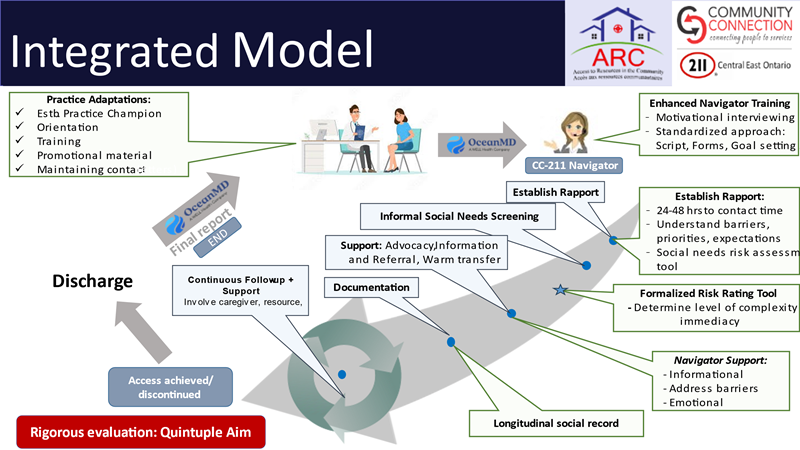
In social prescribing, primary care providers identify patients who have unmet non-medical health and social needs, engage them in addressing these needs, and connect them with a patient navigator who will help access the right resources or programs. For example, a patient navigator may help a single mother who doesn’t have sufficient income for medications enroll in the Ontario Drug Benefit program, or they may connect a patient with poorly controlled diabetes to a subsidized gym membership, free dietary counselling or local diabetes management program.
The first and only Canadian randomized controlled trial of social prescribing – the Access to Resources in the Community (ARC) – which was funded by an OSSU IMPACT Award and conducted in East Ottawa and Sudbury, showed the value of this approach. These two regions have high densities of francophones living in a minority situation. The trial demonstrated that this innovative, patient centered, bilingual navigation services have positive impact on equitable access to needed resources and patient experience. ARC has partnered with Community Connection 211 to expand this much-needed approach in other parts of the province.
The program shows great promise and received a shout-out from the deputy minister of health at OSSU’s Research Day earlier this fall.

“It’s very exciting that the deputy minister mentioned our program at the OSSU meeting,” said Dr. Simone Dahrouge, a researcher at Bruyère Research Institute and lead of ARC.
“ARC was a grassroots program to address a care delivery gap in the Ottawa region, and unbeknownst to us, we were developing a social prescribing program. Social prescribing was not yet known in Canada,” she said.
Her team approached Community Connection 211 in Collingwood, which had piloted a social prescribing program, to work together to integrate learnings, standardize tools and training to grow a scalable model.
For many people, the patient navigators at the end of the phone offer a sympathetic ear as well as links to community resources.
“We take time with clients, through multiple phone calls, to understand their needs and identify any barriers they are facing. Social needs are often interdependent, clients who cannot afford medication may be eligible for programs that could offset utility payments, for example. Understanding what risk level people are at also helps us to prioritize the programs they need,” said Pamela Hillier, Executive Director, Community Connection in Collingwood.
“The navigator provides a lot of emotional support to the patient, and that has come out as really valued,” said Dr. Dahrouge. “With active listening, the patient feels heard and develops trust with the navigator, and is more likely to follow through with acting on their need.”
211 is a national dialling code for navigation services that provide information on available resources and use an extensive database of resources to locate and refer the patient to the appropriate services. However, as patients must call 211 to receive the service, support consists of a single encounter, and because 211 is anonymous, the navigators cannot view a client’s history or status. This limits a holistic understanding of clients with more complex challenges. The team used the analogy of a walk-in clinic versus having a family doctor.
Community Connection is one of five 211 service providers in Ontario. To better serve vulnerable populations, they developed a social prescribing eReferral program with the Georgian Bay Family Health Team in 2015. The program has expanded to receive eReferrals from ten family health teams, several hospitals and paramedic and paramedicine programs. The program is based on trauma-informed principles and includes social needs assessments that measure change over time.
What’s next?
The team of researchers and their non-profit partner are developing a scalable, bilingual, patient-centered social prescribing model by combining attributes of the ARC model with innovative technology that Community Connection 211 is embedding in their navigation record. In 2024, they plan to introduce, and evaluate, this social prescribing program in two Ontario Health Teams in the Ottawa region which are keen to adopt such a model.
“I want this to be the single point of entry for any health or social issue for all patients,” said Dr. Dahrouge. “We especially want to reach the people who are less well connected, have lower health literacy, and in general need help to address their non-medical needs.”
Sounds like just what the doctor ordered.